WAP vs. MAT on ECG: What’s the difference?
The wandering atrial pacemaker and multifocal atrial tachycardia:
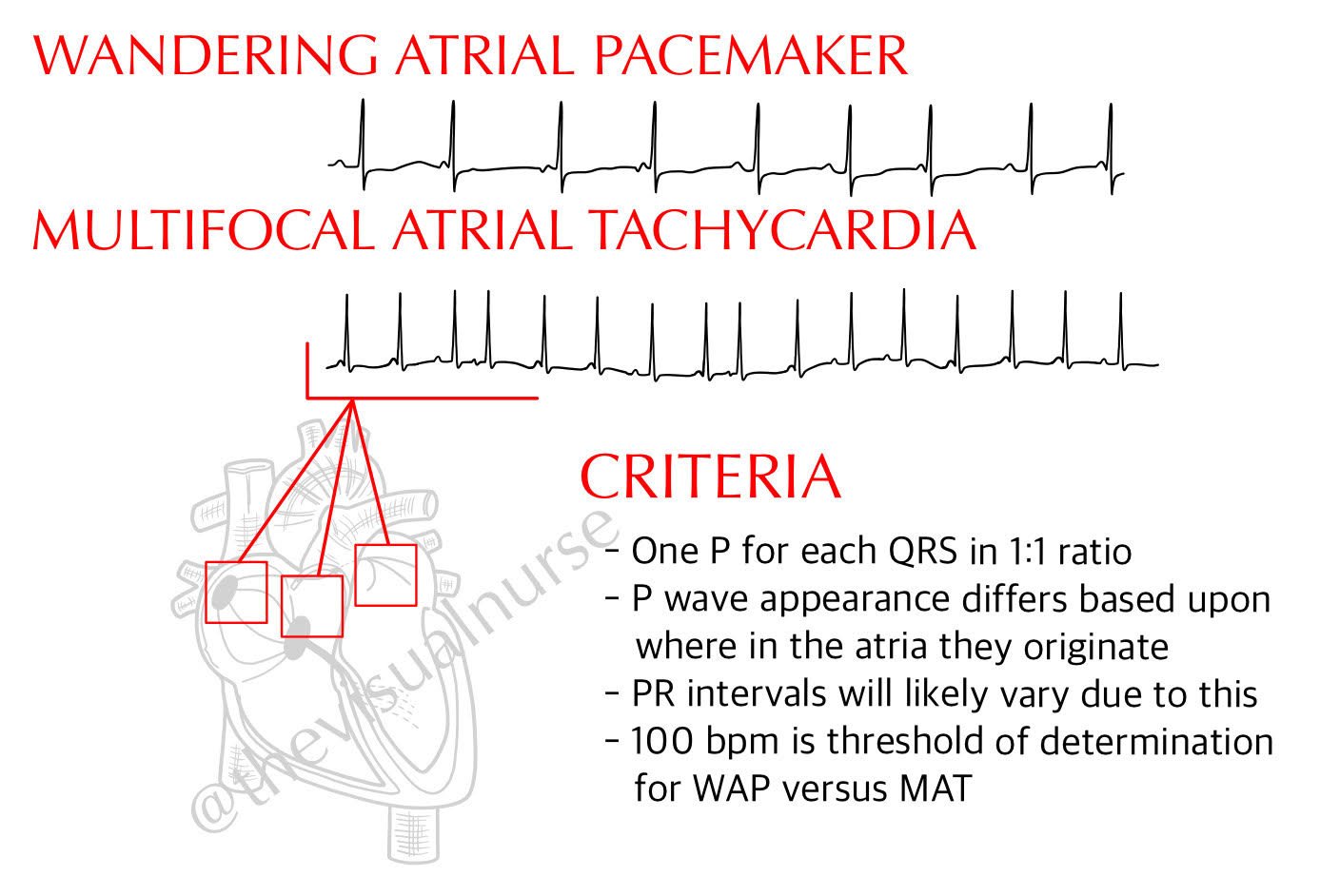
For our purposes, think of these two rhythms as one in the same. The only difference? Heart rate. Is it above or below 100 beats per minute? If it’s less than 100 BPM, you’re looking at WAP. Greater than 100 BPM? You’re looking at MAT.
The wandering atrial pacemaker has nothing to do with extrinsic cardiac hardware.
The sino-atrial node is the natural pacemaker of the heart. Remember also that if P waves all appear similar and they’re arriving at a rate of 60 – 100 beats per minute we assume them to be sinus. Why? My P waves may not look like your P waves. But if all of my P waves look the same, they’re said to have the same morphology. And if they have the same morphology, they’re very likely coming from the same site. But what if the morphology of the P wave is changing? Would that mean that it’s coming from a different site?
This is exactly what happens in the case of the wandering atrial pacemaker. The pacemaker, the site is setting the pace for the rate of the heart, is wandering throughout the atria. This isn’t entirely true... It’s not travelling necessarily, but it describes a case in which there are multiple sites in the atria that are discharging and effectively competing to become the natural pacemaker. This results in at least three different P wave morphologies, and often the PR interval may vary due to this. If the heart rate is less than 100 BPM we call this a wandering atrial pacemaker, or WAP. If it’s greater than 100 BPM we call it a multifocal atrial tachycardia, or MAT for short.
Causes of WAP and MAT might include lung diseases, oxygenation deficiencies, electrolyte abnormalities, stimulant use and others (and may be a transitional rhythm between frequent PACs and Afib). Wandering atrial pacemaker is largely a benign rhythm. If the rate is too high (MAT), treating the underlying cause is typically the first step with rate controlling medications playing a role if needed.
Hope this helps!
- Tyler